April 2021
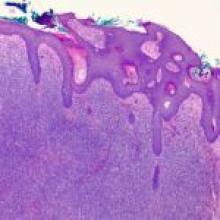
A 68-year-old woman presented to the emergency department after a family member checked on the patient and found her in unlivable home conditions. Once she arrived at the emergency department, the patient had no acute complaints, but had a large, masslike open wound that covered the upper half of the patient's face/forehead with noted infestation of maggots on the infected skin.