September 30, 2021
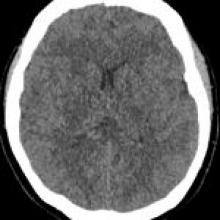
A 63-year-old woman was found unresponsive and in respiratory arrest following attempted suicide by self-asphyxiation. She was intubated and admitted directly to the ICU. MRI was performed 10 days into ICU admission due to abnormal cognition during weaning off sedation. Previous intracranial MRI, performed during an unrelated presentation, had been normal.